Any kind of surgery is an invasive process which puts considerable stress on the body. In particular, the cardiovascular, respiratory, excretory and immune systems are put at risk and the body’s ability to maintain homeostasis is compromised.
Therefore, if surgery is necessary, using minimally invasive surgery (MIS) techniques to limit the size and number of incisions made is a real benefit to the patient.
There are many advantages of MIS over traditional open surgery. The wounds caused by MIS procedures are smaller which helps shorten recovery times as well as leaving less noticeable scars. As patients recover more quickly, they can leave hospital sooner, freeing up hospital beds for other patients. For many patients using MIS results in them experiencing less pain and, as a result, needing less medication post-surgery.
Analyst firm Market & Markets predicts that by 2025, the global business for MIS-related equipment will be worth approximately $32.7 billion annually. The specialist fields where it is proving of particular value are in thoracic, orthopaedic, urological, vascular, gynaecological and neurological surgery, as well as interventional cardiology.
The pioneering work that led to modern-day MIS began back in the early 1980s, with the introduction of various types of electro-surgical instruments (catheters, endoscopes, laparoscopes, arthroscopes etc) being pivotal in its on-going technological progression. Now, it is estimated that over 90% of all surgical activity can be performed using MIS. These activities include appendectomy, tubal ligation, cholecystectomy, gastric bypass/banding, heart valve repair, myomectomy, hysterectomy, arthroscopy, prostatectomy, spinal fusion and bariatric procedures. In the future, surgeons will be able to make even greater use of MIS, as the supporting technology becomes increasingly sophisticated.
Compact form factors
Ongoing innovations in electro-surgical instruments will enable the incorporation of elevated levels of functionality and, consequently, these instruments will be more effective.
Opportunities will also open up for MIS to be applied to the treatment of a broader spectrum of health conditions and medical complaints.
However, to retain their ‘non-invasive’ properties, the surgical devices used for procedures must be in the most compact of form factors. This has far-reaching implications for the constituent electronics – not just in terms of the component parts (micro-sensors, micro-sensors, actuators, power management ICs, etc.) – but also for the wiring that delivers the data signals and power to them.
Traditionally, the wiring involved in these designs has not been much of a concern in terms of the space it takes up. Demands to shrink form factors yet simultaneously add more functional elements is placing exacting space constraints onto instrument designs.
The current approach to how medical devices are wired will need to change.
Until now, conventional electro-surgical instrument designs have relied on electrical interconnects that are based on microwire technology where wires usually need to be combined together into bundles around 600µm in diameter.
Beyond their thickness, microwires have other shortfalls that medical engineers should be aware of, such as rigidity, as this makes them less easy to apply to enclosure formats that have unusual shapes.
As the density of the electronic content packed into modern electro-surgical instruments keeps increasing, the interfaces connecting everything together will need to evolve accordingly.
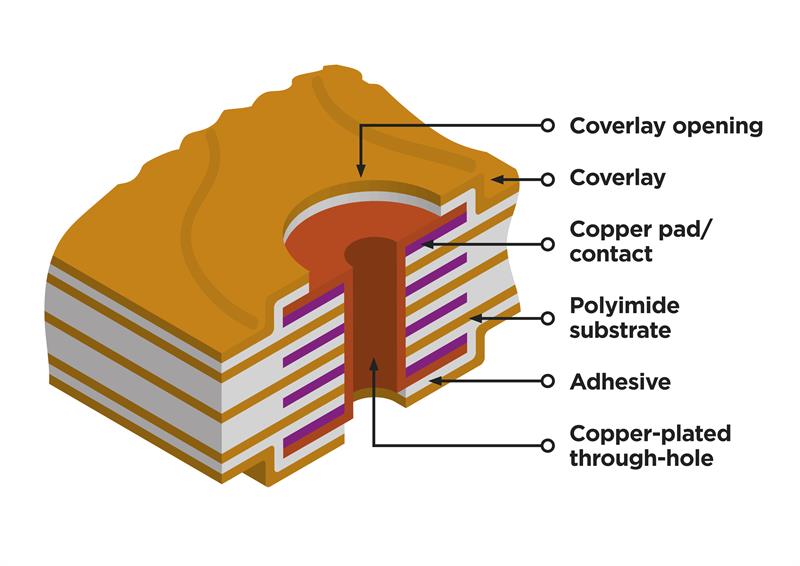
Flexible printed circuits (FPCs) are a viable option for supplanting microwires as they offer substantial space and weight savings while still supporting high degrees of signal integrity and prolonged operational reliability.
Because of these attributes, FPCs have already seen widespread uptake in an array of wearable and implantable medical devices used for the monitoring, regulation and assistance of vital physiological processes like pacemakers, hearing aids and blood glucose monitors.
Other advantages are their ability to be bent and shaped in order to fit the dimensions of the enclosure they are contained within. The composite structure of FPCs gives them considerable mechanical robustness, so they can operate effectively whilst in fact being significantly thinner.
By using an FPC, it is possible to implement conductive traces that are just 25μm wide. With a total interconnect thickness (including the accompanying electrical insulation and protective layers) that is less than 50μm, this solution is slightly thinner than the average human hair. Therefore, a single FPC can replace up to 12 microwires – not only curbing the space taken up, but reducing the complexity of the instrument’s wiring assembly too. It should also be noted that there are additional cost savings to factor in: since multiple microwire interfaces can be replaced by a single FPC, a reduction in the bill-of-materials and in the outlay on product assembly is possible.
Above: An example of an ultra-thin IHT interconnect
Manufacturing issues
Though FPCs present an attractive alternative to microwires, there is still one major obstacle to overcome if they are to be mass produced and designed into devices for MIS procedures.
Manufacturing techniques have put constraints on the FPC lengths that it is possible to manufacture. In most cases, most FPC manufacturers have only been able to support lengths of around 0.6 metres, with just a few companies capable of offering solutions of around 2 metres.
This has undoubtedly had a detrimental effect on their ability to address medical devices OEMs’ design criteria.
To put it simply, there are a multitude of MIS application scenarios where longer wiring solutions are necessary. For example, catheters used in cardiac procedures will need to have a minimum length of 1.1m if clinical staff are to be able to use them correctly. Likewise, for procedures such as interventional neuroradiology, 2m wiring lengths are required.
Through its proprietary Improved Harness Technology (IHT), Trackwise is now in what can truly be described as a unique position in that it can manufacture multi-layer FPCs of any length. This manufacturing breakthrough gives OEMs serving the medical sector a lightweight, space-saving, length-unlimited alternative to current solutions.
Unlike conventional approaches to FPC production, IHT employs a fully patented dynamic process which is based on advanced roll-to-roll electro-lamination techniques.
By using these techniques, it is possible to create FPCs that can meet any length requirement, ensuring ongoing reliability and repeatability, while keeping the associated unit costs down. The planar nature of IHT interconnects allows them to be bonded within the structure they are mounted to, reducing the physical space that they occupy.
Thanks to IHT, Trackwise has the scope to produce FPCs of far longer lengths than are available from other sources – allowing medical OEMs to gain access to a cost-effective, high-volume supply of FPCs that are suitable for their specific application demands.
This is certain to be of value as the next generation of MIS instruments is designed and introduced.
Author details: Philip Johnston is CEO, Trackwise













