Sleep apnoea is a serious sleep disorder that occurs when a person’s breathing is interrupted during sleep. Untreated, those with the disorder stop breathing repeatedly during their sleep and this can happen hundreds of times over a 6 to 8 hours sleep cycle.
When a person stops breathing, the brain – and the rest of the body – may not be getting enough oxygen.
Potentially life threatening, sleep apnoea is far more common than previously thought. It happens in both genders and all age groups. It is estimated that about 25% of men and nearly 10% of women suffer from it and it can affect people of all ages, including infants, but it’s more common in those over 40 and overweight.
According to the Cleveland Clinic, there are two types of sleep apnoea: obstructive and central.
Obstructive sleep apnoea is the more common and occurs as repetitive episodes of complete or partial upper airway blockage during sleep. During an apnoeic episode, the diaphragm and chest muscles work harder as the pressure increases to open the airway. Breathing usually resumes with a loud gasp or body jerk. These episodes can interfere with sound sleep, reduce the flow of oxygen to vital organs, and cause heart rhythm irregularities.
In central sleep apnoea, the airway is not blocked but the brain fails to signal the muscles to breathe due to instability in the respiratory control centre. Central apnoea is related to the function of the central nervous system.
If it’s not treated, sleep apnoea can cause several health problems, including hypertension (high blood pressure), stroke, cardiomyopathy (enlargement of the muscle tissue of the heart), heart failure, diabetes and heart attacks.
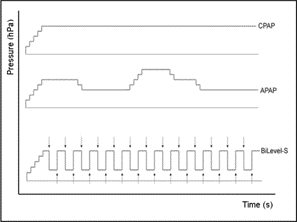
Figure 1: Example of pressure patterns of CPAP vs. APAP vs. BiPAP (source: NIH)
Positive Airway Pressure therapy, or PAP therapy, is the most common treatment for obstructive sleep apnoea. With PAP therapy, patients wear a mask over their nose and/or mouth and an air blower gently forces air through the mask.
The air pressure is adjusted so that it is just enough to prevent the upper airway tissues from collapsing during sleep. PAP therapy prevents airway closure while in use, but apnoea episodes can return if PAP is stopped or if it is used improperly. Properly used, PAP helps patients breathe and maintain good blood oxygen levels throughout the night.
There are three main types of positive airway pressure devices depending on specific needs of the patient:
CPAP (Continuous Positive Airway Pressure). CPAP is the most common type of machine. This device is programmed to produce pressurised air at one steady air pressure level. To change the air pressure, you must reset the device’s settings. If the patient needs more or less pressure during the night, the CPAP is not able to adjust.
BiPAP (Bi-Level Positive Airway Pressure). BiPAP machines have two pressure settings, one pressure for inhaling and a lower pressure for exhaling. It’s used for individuals who can’t tolerate CPAP machines or have elevated carbon dioxide levels in their blood. BiPAP devices can also come with a backup respiratory rate for patients who have central sleep apnoea. The backup respiratory rate ensures the person breathes, as the main problem with central sleep apnoea is initiating breath. BiPAP is also helpful for other conditions affecting the lungs, such as COPD.
APAP (Automatic Positive Airway Pressure). APAP machines check a patient’s breathing throughout the night. They automatically adjust the air pressure to compensate for changes in sleep position or the effects of medications that may have changed breathing patterns. Unlike CPAP machines, APAP machines can automatically choose the right pressure setting based on a patient’s breathing needs. This allows for much greater flexibility.
PAP machines include several types of sensors to monitor and/or regulate different functions, including airflow, air pressure, temperature and humidity. While adjusting temperature and humidity is important for the patient experience, two key functions are served by pressure sensors: airflow and air pressure.
A gage pressure sensor is used to monitor the patient’s airflow. Specifically, airflow sensors monitor the patient’s breathing and send a signal to the machine to reduce the system airflow when a patient exhales and then increase it again when the patient inhales.
Adjusting the system airflow when inhaling and exhaling results in the patient being much more comfortable as he/she is no longer ‘fighting’ against the sleep apnoea machine when exhaling. The most effective airflow sensors have a very fast feedback loop (to tell the system to adjust the fan more quickly when a patient is inhaling/exhaling), are able to effectively block out noise from fans and motors (to reduce error rates), can support multiple pressures without any degradation in performance and have a high-resolution rate to ensure a very strong signal-to-noise (SNR) ratio.
Figure 2: NimbleSense Building Blocks that Benefit PAP Machines
A differential pressure sensor is used for system flow measurement. While the gage sensor monitors the patient’s breathing, the differential sensor monitors the sleep apnoea machine to ensure it is providing the right amount of pressurised air from the device to the patient. Just as with measuring patient airflow, the most effective system flow measurement sensors have a very fast feedback loop (to more accurately report the flow of pressurised air), are able to effectively block out noise from fans and motors (to reduce error rates), can support multiple pressures without any degradation in performance (depending on the patient, a different flow rate may be required) and have a high-resolution rate to ensure a very strong signal-to-noise (SNR) ratio.
Having an extremely low noise floor, the NimbleSense architecture has been developed for the precise, low-pressure measurements that PAP equipment requires to maximise their accuracy and performance.
In addition, Superior Sensors – a developer of advanced sensors - has gone a step further with its CP Series by integrating the two pressure sensors (gage and differential) in one device. This highly integrated dual sensor solution eliminates the need of a second pressure sensor. Finally, several application-specific building blocks provide additional capabilities to further improve the sleep apnoea solution. These include Multi-Range Technology, an advanced multi-order filter and integrated closed loop control.
Integrated Dual Pressure Sensor Solution
Utilising the same small package as with single sensor solutions, the CP Series is the industry’s first fully integrated dual pressure sensor solution that also provides 64 possible configurations. By combining the two sensors in one device, PAP product design is simplified, time to market accelerated, PCB space requirements reduced, and overall system costs lowered.
The NimbleSense architecture was developed with the overarching goal to knock out every bit of noise before reaching the sensing system. This provides a much better SNR that competing solutions for both gage and differential pressure sensors. The net result is that both integrated sensors boast accuracy that is within 0.05% of the selected pressure range, total error band (TEB) within 0.15% of FSS and long-term stability within 0.15% of FSS per year.
As part of its enhanced performance, the CP Series has a very fast 2 millisecond response time. This ensures that both sensors are providing timely feedback to the PAP machine, resulting in maximum patient comfort and machine efficiency.
Unprecedented Flexibility
With one product SKU, you can support up to 64 possible configurations with your PAP machine. This provides maximum flexibility and the ability to quickly manufacture derivative products to expand a portfolio of products. Each of the two pressure sensors has 4 factory calibrated pressure ranges. In addition, there are four bandwidth filter options that can be selected. This level of flexibility is said to be a first with pressure sensors for sleep apnoea devices.
The CP Series also comes with several additional features that can be integrated into the sensor. An advanced multi-order filter can be implemented to further reduce any interference coming from fans or blowers. This eliminates noise before it can become an error signal. In addition, an integrated closed loop control can be implemented to significantly reduce loop delays by controlling the fan/blower. Integrating these optional features will further simplify product design and improve system performance.
Conclusion
Potentially life threatening, sleep apnoea is a serious disorder that affects hundreds of millions of people. PAP therapy is the most common and recommended treatment sleep apnoea, and PAP machines rely on pressure sensors to monitor both the airflow of the system and the patient’s breathing.
The CP Series of highly integrated sensors combines the two pressure sensors in one device to simply product design and reduce system cost, while the NimbleSense architecture provides improved performance, faster response times and maximum flexibility with 64 possible configurations from one SKU.
Author details:
LCDTek is a distributor of standard and custom displays, module and embedded solutions.













