Continuous airflow measurements during anaesthesia monitoring, intensive care treatment as well as in clinical and ambulatory environments provide important information for the assessment of cardiorespiratory and breathing circuit behaviour and have become indispensable in modern medicine.
Mechanical ventilation systems supply patients with breathing gas by means of mechanical “air pumps” and this ventilation technique uses positive pressure to deliver air to the patient’s lungs.
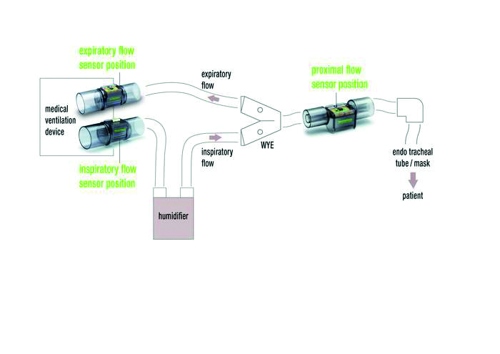
Figure 1: Schematic construction of a ventilator with the typical different sensor positions and the use of a humidifier.
The increase of intelligent features incorporated into these ventilators, allow them to automatically adapt to changes in lung function or patient breathing. Modern pressure-controlled or volume-controlled ventilation is therefore now more patient oriented than ever. Since fewer and fewer ventilation modes are required due to the increase in device intelligence, medical ventilators have overall become less complex to operate.
Non-invasive ventilation refers to ventilation therapies that are performed using masks or nasal cannulas. This is often referred to as mask ventilation or NIV/NPPV (non-invasive ventilation or non-invasive positive pressure ventilation). In invasive ventilation, an endotracheal tube or a tracheal cannula is inserted into the trachea of the patient to supply the lungs with air. Both types of ventilation – non-invasive and invasive – have merit and are used in a complementary manner.
A factor that should not be underestimated is the humidification of the inhaled air as it goes far beyond mere patient comfort. Well-humidified and warmed air contributes significantly to the success of ventilation therapy as it improves both secretion drainage and the tolerance of non-invasive ventilation therapy.
Current trends in hospitals show that non-invasive ventilation is used more frequently today and for far more symptoms than ever before. Intensive care units, for example, increasingly use non-invasive ventilation as a first-line of treatment, which reduces infectious complications, weaning periods, ICU stay lengths, intubation rates and costs.
The key issue for all ventilators is the accurate measurement of the breathing gas flow rate and the volume of breathing gas that flows in and out of the patient. These measurements with the highest sensitivity and accuracy enable the previously mentioned and nowadays prevailing patient-oriented ventilation, which also better reflects the pathophysiology of the patient. Figure 1 shows the schematic construction of a ventilator with the typical air flow/sensor positions.
Technical challenges
The complex breathing circuits have a wide range of composition variability due to the different types of tubing, humidifiers, filters and adapters used. This often results in leaks and imperfections, which is why the inspiratory flow rate (I) sometimes differs significantly from the flow rate that actually reaches the patient. The same applies to the expiratory flow rate (E). Airflow measurements are also hampered by the constant changes in air temperature, humidity and breathing gas composition as well as the contamination of hoses and expiratory/proximal sensors with sputum, pathogens and blood. Due to technical limitations, measurements of inspiratory (I) and expiratory flow rates (E) were performed inside the ventilator in the past. The rough flow values were then corrected as far as possible using complex and often inaccurate compensation algorithms.

Figure 2: Proximal sensors (single-use and reusable) for adult ventilation.
Proximal sensors
Originating from neonatology, it is accepted that the best measurement position for patient airflow, volume and pressure measurements is as close as possible, i.e., proximally (P), to the patient. This allows patients to be ventilated with a tidal volume that is as accurate as possible and the effects of the ventilation circuit composition mentioned above are almost entirely eliminated. Additional advantages of proximal flow measurement are the instant detection of respiratory signals, to which the ventilator can respond even faster, as well as the detection of leakages. Particularly for reducing the effect of leakages proximal sensors prove helpful in both volume-controlled and pressure-controlled ventilation and help reduce the causes of monitoring and triggering problems.
The continuous development of ventilators has always been linked to the available sensor technology. A next generation development of the hot wire anemometer is the Sensirion CMOSens Technology, which is used in Sensirion mass flow sensors and differential pressure sensors. With the CMOSens Technology, Sensirion has developed a sensor range based on MEMS technology that now covers all the modern ventilator sensor requirements:
- Inspiratory sensor solution (I) for accurate and instant fan control and inspiratory airflow monitoring
- Expiratory sensor solution (E) for balancing the air exhaled by the patient with inspiratory ventilated air
- Proximal sensor solution (P) to measure inhaled and exhaled air directly at the patient with the highest accuracy
Next-generation technology
Some of the key differences to its predecessor technology, hot wire anemometers, are that the modern flow sensor solutions deliver a digital, fully calibrated and temperature-compensated output signal. The sensors can be directly used with the patient and thus without prior time-consuming or periodically required recalibration. Furthermore, the sensors allow to measure airflow symmetrically in both directions. The robust sensor technology does not require zero-point adjustment, does not drift over time and does not need to be calibrated during the life-time of the sensor. The technology also allows hysteresis-free and position-independent use with a dynamic measurement range and a high measurement sensitivity at all flow ranges. Since the measurement signal is processed directly inside the sensor and the output is digital and temperature compensated flow values, no further costly components such as A/D converters are required. All these benefits enable the medical staff to safely, easily and quickly as well as reliably manage patient ventilation, which provides significant advantages when it comes to challenging emergency ventilation as well as in subacute care and home care settings.
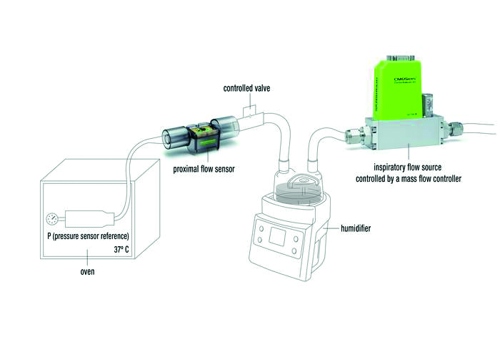
Figure 3. Schematic of a ventilation setup with extremely humid air and a very small tidal volume of only 5 ml.
Proximal flow sensors must be reliable and cost effective, long-term stable and, moreover, feature numerous other ventilator-specific features in order to be suited for modern patient-oriented ventilation. In addition, particularly stringent requirements for hygienic sterilization are needed as the sensors come into contact with air that is potentially contaminated with pathogens.
The Achilles’ heel of all current air flow sensors is the use in combination with humidifiers. High humidity becomes a problem when it leads to condensation, causing macroscopic water droplets to rain out in in the cooler parts of the ventilator circuit. As a solution, all Sensirion proximal and expiratory sensors are equipped with an additional external heating element. Operation of this heating element with a maximum of 0.5 W is sufficient to reliably prevent condensation in the sensor and thus ensure long-term stable and reliable operation.
The schematic illustrated in Figure 3 shows a humidifier typically used in ventilator setups to ensure the breathing air is well humidified. The steel cylinder in the oven is kept at 37°C and simulates the lungs with the connected pressure sensor used as a reference. The controlled valve is closed during the inspiratory breathing cycle and opened once per second for the expiratory part of the breathing cycle.
Without the use of the heater, individual drops of water can run over the sensor element and cause misreading of the measurement values. This misreading can clearly be recognized by the deviations of the expiratory/inspiratory volume from the reference volume.
Outlook
The use and spread of ventilators will continue to grow strongly in the future due to the increasing number of lung diseases. Modern ventilators place ever-growing demands on sensors in order to place the focus on the patients and their therapy.
The CMOSens Technology has established a new generation of flow sensors that have proven their reliability millions of times in the field of CPAP devices and automotive applications with the advantages for ventilators being evident.
It is the technological advantage that will enable manufacturers to realise the next quantum leaps in ventilation.
Author: Andreas Alt is Sales Director Medical Sensirion AG













