According to the ONS, approximately 22% of all UK deaths in 2018 were considered avoidable. Of these, 64% could be attributed to causes considered preventable and 36% to treatable conditions. Improving the diagnostic process is therefore one of the most important areas where AI is being implemented.
For example, incomplete medical histories and large caseloads can lead to serious human error. Immune to human error, AI can predict and diagnose disease faster than most medical professionals. In one study, an AI model using algorithms and deep learning diagnosed breast cancer at a higher rate than 11 pathologists.
“Healthcare at every level is dependent on algorithms of one kind or another,” said Parashkev Nachev, Professor of Neurology, Brain Repair and Rehabilitation at UCL Queen Square Institute of Neurology. “They are needed to ensure care is reproducible, objective and scalable. What I'm trying to do is maintain these characteristics while introducing greater complexity, so care can be better tailored to individual patients.”
This means that when you present to your doctor, your treatment is informed not by the average of the population – from which you may be very distant – but by the “neighbourhood” of people like you, those whose characteristics are most similar to yours.
He adds that these ideas can also be applied to how hospitals are run. For example, the UCLH’s work on non-attendance, which drew intelligence from complex algorithms in order to work out which patients were more likely not to attend their appointment and remind those who need to be reminded.
Prof Nachev said, “The objective was to increase the yield of reminding interventions so that the fewest number of patients missed their appointments, ensuring consequent delays to care are minimised. Already established at UCLH, it is an approach that others, such as DrDoctor, are helping disseminate across the NHS.”
Diagnosing and reducing error
The NHS Accelerated Access Collaborative (AAC), chaired by Lord Ara Darzi, aims to make the UK one of the most pro-innovation health systems in the world by pooling the knowledge and expertise of its board members who represent various departments across the NHS, government, and industry.
The AAC runs the Artificial Intelligence in Health and Care Award in partnership with NHSX and the National Institute for Health Research. The award will make £140 million available over three years to accelerate the testing and evaluation of promising AI technologies – from initial feasibility to evaluation within the NHS.
The winners of the first round of the competition were announced on the 8th September 2020.
Among them were Oxford University spin out, Brainomix’s ‘e-Stroke suite’ - a collection of tools that use state-of-the-art AI algorithms that provide real-time interpretation of brain scans to help guide treatment and transfer decisions for stroke patients.
Another was RITA (Referral Intelligence and Triage Automation), Deloitte’s solution that automates the triage of GP referrals by reducing the administrative burden on healthcare professionals by assessing the urgency of referrals.
Dutch company, Aidence, has developed Veye Chest, an AI platform to optimise oncology pathways, to automate early lung cancer detection.
Healthy.io’s home test kit and mobile app allows patients to self-test at home with clinical grade results. Integrated into the Electronic Medical Record (EMR), real-time results are available for clinicians to review and follow-up. Shifting to testing at home is said to increase uptake, improve quality, reduce workload in primary care, and create savings.
Deep learning software has been developed by Kheiron Medical Technologies to solve critical challenges in the NHS Breast Screening Programme, including reducing missed cancers, tackling the rising shortage of radiologists and improving delays that put women’s lives at risk.
DLCExpert by Mirada Medical uses AI software to automate the time-consuming and skill-intensive task of outlining (or ‘contouring’) healthy organs on medical images for radiotherapy planning so that they are not irradiated during treatment.
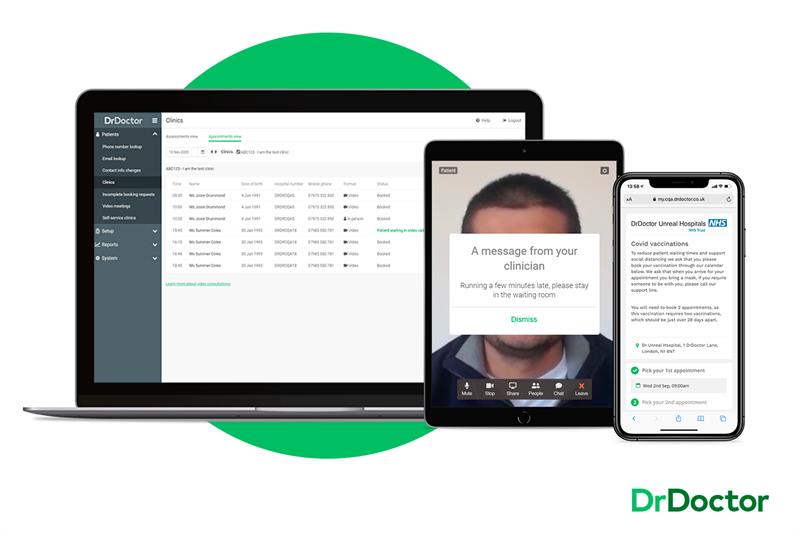
ICNH’s DrDoctor deploys AI to obtain the greatest use from every scheduled appointment within a hospital. It ensures attendance is as high as possible by using past appointment attendance and demographic data to predict those less likely to attend in future and customising communication with these demographics accordingly.
The AAC is now working with these companies to finalise which site they will be selected for use at and match them to appropriate NHS healthcare services to support testing for each product. It will also evaluate where appropriate evidence is collected to enable faster roll-out of these AI innovations into the NHS.
Streamlining patient experience
Time is money. Efficiently providing a seamless patient experience allows hospitals, clinics and physicians to treat more patients on a daily basis. AI is streamlining the patient experience, helping hospital staff process millions, if not billions of data points, faster and more efficiently.
Netta Myrhinen, head of communications at DrDoctor, explained, “We took patient demographics and used this data to find out why some people turn up, and why some don’t. The data we received helped us work out who needs to be sent extra reminders, or bespoke communication, or who needs a closer touch point with the hospital so that they stay engaged.
“We found that men in their early 20s are the least likely to keep an appointment. This could be, for example, that they’ve moved away from home for the first time, perhaps they're in university and their parents used to sort out their appointments.
“We can now send them a reminder that says ‘let us know and we can find you a time that suits you’, to give them that control, not just tell them that they have to come in.”
Guys & St Thomas hospital in London achieved a 25% reduction in DNA (did not attend) rates via DrDoctor’s appointment management solution – which equates to £2.6m in savings per year.
At the Royal Orthopaedic Hospital (a smaller, more specialist Trust with an entirely different patient demographic), DrDoctor achieved a 35% reduction in DNA equating to £100,000 savings annually.
Myrhinen adds: “There is huge potential to improve upon these results once AI is employed in decision making. By using machine learning to predict who should be sent additional communication (such as an appointment reminder) it is possible to ensure that clinic utilisation is optimal and patients that need care actually receive it.”
Further funding
Prof Nachev says that for AI to work most effectively in healthcare applications, three things are required: safely accessible data of adequate scale and inclusivity, complex algorithms that can deal with the immense heterogeneity of clinical data, and as much compute capacity as possible. The last is often neglected.
He said, “If you gave me a 400 petaflop machine, such as the Cambridge-1 AI Supercomputer that Nvidia is developing with King’s College London and other partners, I could use all of it even on a single task such as predicting outcomes in stroke. The underlying biology is so complex no model could ever be perfect: only different shades of good. And compute is increasingly the limit on achieved model fidelity.”
He adds that funds being spent in other industries should be matched in healthcare: “The government is planning to buy the Met Office a £1.2billion supercomputer, yet the NHS lacks even modest computing capabilities. If the decision to pick up an umbrella in the morning is so expensively informed, shouldn’t the rather more important decisions taken in hospitals be at least comparably assisted?
“I think the government should think hard about investing more in computation; their focus now appears to be mostly data, and to some extent algorithmics. Without supercomputers we’ll be confined to basic models, and there will be a hard ceiling on what we can achieve.”













